By L. Terry Chappell, T. Rae Neal, Natallie Paphanchith
Incidence and Cost
 Diabetes is a growing epidemic in the United States. According to the National Diabetes Statistics report for 2014, 21 million people in the United States have been diagnosed with type 1 or type 2 diabetes. It is estimated an additional 8.1 million people are undiagnosed. In addition to diabetes, 86 million Americans were diagnosed with the precursor, pre-diabetes in 2012. Treatment and management of this disease is costly. The estimated annual cost of diabetes per year in the US is 245 billion dollars.
Diabetes is a growing epidemic in the United States. According to the National Diabetes Statistics report for 2014, 21 million people in the United States have been diagnosed with type 1 or type 2 diabetes. It is estimated an additional 8.1 million people are undiagnosed. In addition to diabetes, 86 million Americans were diagnosed with the precursor, pre-diabetes in 2012. Treatment and management of this disease is costly. The estimated annual cost of diabetes per year in the US is 245 billion dollars.
More alarming than diagnosis and cost is the impact diabetes has on our overall health and wellbeing. Diabetes was listed as the 7th leading cause of death in the United States in 2010. When diabetes is controlled we reduce the risk of co-existing diseases. Unfortunately, many patients remain with an elevated hemoglobin A1C. Uncontrolled diabetes leads to multiple micro and macro vascular complications. Co-morbidities secondary to diabetes include: hypertension, hyperlipidemia, coronary artery disease, cerebral vascular accidents, chronic kidney disease, amputation, retinopathy, and neuropathy (1).
Conventional Approach to the Treatment of Diabetes
Type 2 diabetes mellitus (T2DM) is clearly linked to obesity. As obesity rates climb, so does the diagnosis. 80-90 percent of patients diagnosed with type 2 diabetes are classified as obese. The International Diabetes Foundation was quoted, “Diabetes and obesity are the biggest public health challenges of the 21st century”. The link here is clear; obesity drives insulin resistance and an inflammatory response. Prolonged insulin resistance puts an extreme amount of stress on the pancreas. When resistance is accompanied by dysfunction of the pancreatic islet b cells that is what ultimately leads to the disease (2).
A dietary goal should be to minimize refined sugars and starches. Modern carbohydrate staples, like potatoes, breads, and cereals, have a high glycemic index (GI) and a very strong link to chronic disease (3). Foods low on the GI scale like sweet potatoes, winter squash, and beans help to stabilize blood glucose levels. This can be achieved with whole structured foods and lower GI. Clinical trials support low GI diets with greater fat content as more effective than low fat diets at preventing complications associated with cardiovascular disease. Often a low fat diet contains the highest GI content, which leads to increased insulin resistance. Low GI diets improved whole body insulin sensitivity throughout the trials with no increase in LDL cholesterol (3). Whole rice and seeds decrease circulating levels of glucose, insulin, LDL cholesterol, and fructosamine, while refined sugar and high fructose corn syrup lead to increased risk for T2DM. Large amounts of fructose result in insulin resistance and could accelerate the development of T2DM and associated complications. Avoiding processed foods is an important step in preventing and managing diabetes (4).
Many treatment options are available to treat diabetes. Since discussing obesity in the previous paragraph, lifestyle modifications are the initial target. Nutritional planning, weight loss and diabetic education are a top priority. However, despite efforts of diet and exercise many patients will require additional therapies. There are multiple oral medications. Metformin is the initial medication of choice if liver and kidney function remain stable. However if the hemoglobin A1C remains elevated after 3 months of therapy an additional agent may be selected. Treatment of diabetes has greatly changed in the last 10 years. Use of Sulfonylureas, Meglitinides and Alpha-glucosidase inhibitors are less common as innovative medications are integrating to the market.
Emerging drug classifications include Thiazolidinediones, DPP-IV inhibitors, GLP agonists, and SGLT2 inhibitors. If insulin resistance remains high and oral medications and injectable non-insulin medications are not effective in maintaining glycemic control, insulin may be added. Likewise, if chronic medical conditions arise and prevent the use of certain medications, a basal bolus regimen of insulin may be more appropriate.
Goals of Treatment
As previously mentioned, treatment goals are targeted by the hemoglobin A1C. The A1C is a 3 month average of the patients’ blood sugar. An A1C less than 5.7 percent is normal, prediabetic range is 5.7-6.4 percent and diabetes is diagnosed if the A1C is greater than 6.5 percent. For patients diagnosed with diabetes The American Diabetes Association recommends an A1C goal less than 7 percent. However, many randomized trails that examined the effects of glycemic control excluded the frail elderly (5).
Newer data points to higher health threats in the elderly population with tight glycemic control. The most common risk is severe hypoglycemia. Hypoglycemia leads to increased falls, injury, trauma, and hospitalizations (6). Also, elderly patients are more likely to experience adverse effects from their medications. The American Geriatric Society recommends the targeted A1C to be 8% in the elderly (7). However, the A1C target is controversial among various organizations. Ultimately, goals should have an individualist approach and target.
Complementary Treatment Options and Lifestyle Measures
Complementary, alternative, integrative, or comprehensive, whatever term you choose, these additional approaches to medicine offer many options for the prevention and treatment of T2DM. The California Institute of Integral Studies and Integrative Medicine presented a paradigm shift in our health care system at the International Congress for Clinicians in Complementary and Integrative Medicine in 2013 (8). Collaborative practice and interaction between disciplines will provide valuable insight toward a new health care model. It is estimated that as much as 40% of adults use complementary and alternative medicine (CAM) with up to 34% of those patients having a chronic disease. These figures are deceptive when disclosure of CAM use is often withheld due to conflict with other providers (9).
Personal responsibility is essential for prevention and management of diabetes. Awareness of recommended caloric intake and ideal body weight prevent the buildup of excess body fat, which can lead to cellular insulin resistance. Maintaining ideal body weight and modifying the diet to include important nutrients, limit less beneficial ingredients, and eliminate harmful options will lead to improved glycemic control(4). Organic pollutants also accumulate in adipose tissue and carry destructive consequences. Sorbitol accumulation caused by environmental exposure leads to cell death and contributes to diabetic complications (4). Weight loss and detoxification will improve insulin sensitivity and glucose tolerance. Losing as little as 5% of body fat leads to marked improvement in glycemic control and reduces the incidence of T2DM by up to 50% (10).
Gaby also identified a gluten free diet as delaying or preventing the development ofT2DM due to the preservation of beta cells. Vegan diets improve glycemic control. Coffee is associated with a decrease risk of developing T2DM. Oolong tea is associated with a mean decrease in plasma glucose concentrations. This could be due to reducing iron absorption, which might improve glycemic control. Modest increases in body iron stores have an adverse effect on glucose metabolism. Iron depletion enhances glucose utilization. Phlebotomy treatments have effectively reduced iron concentration to vegetarian levels and caused a 40% increase in insulin sensitivity (4). Deferoxamine, an iron-chelating agent, was used in poorly controlled diabetic patients with elevated ferritin levels successfully to improve blood glucose and HbA1c levels (4).
Increased dietary fiber from legumes, carrots, artichokes, peaches, strawberries, and grapefruit can improve glycemic control. Obtaining fiber from food is preferred. If supplementation is necessary, unprocessed wheat bran or apple fiber are recommended. Legumes have an ability to flatten blood sugar response for over four hours, when eaten at breakfast. The blood sugar remained consistent four hours after ingestion (4).
The temperature and manner in which food is cooked plays a role in the development of diabetes. The advanced glycation end products (AGE) remain in food after the cooking process. These products cause modifications in protein structure, which promote inflammation (4). Less AGE formation results from cooking techniques using water at low temperatures for a longer period of time. An emphasis on boiling, poaching, and stewing over frying, broiling, and roasting can decrease AGE by up to 50%. AGE products play a role in the pathogenesis of insulin resistance and diabetic complications (4).
Effect of acidic environment on the advanced glycation end product (AGE) content of beef. Beef (25 g) was roasted for 15 minutes at 150°C with or without premarinating in 10 mL vinegar (A) or lemon juice (B) for 1 hour. Samples were homogenized and AGE (Nε-carboxy-methyl-lysine) content was assessed by enzyme-linked immunosorbent assay as described in the Methods section. Data are shown as % change from raw state. White bars represent raw state, hatched bars roasted without marinating and black bars marinated samples. *Significant changes compared to the raw state (P<0.05). #Significant changes compared to cooked without marinating samples. 1=raw beef. 2=roasted beef with no vinegar or lemon. 3=roasted beef after marinating with either vinegar or lemon for 1 hour.
Consuming raw fats such as sesame, coconut, avocado, flax seed and olive oil help to reduce HbA1c. Esposito et al. found that a low carb Mediterranean diet effectively reduced HbA1c, achieved diabetes remission, and delayed the need for medications (11). Harokopio at the University of Athens found eating plenty of olive oil, fish, and whole grains was more effective at slowing the progression of T2DM than a low fat diet. The key factor in the Mediterranean diet is that more than 30% of daily calories are from fat. Olive oil is high in oleic acid and monounsaturated content providing antioxidant and anti-inflammatory properties (12).
Mind body medicine, recognized by the National Center for Complementary Medicine, includes, yoga, Tai Chi, and meditation. These techniques are used to influence the mind body connection. Movement, breathing, meditation, and chanting can be used to achieve life style changes, stress relief, and allow inner focus. The American Diabetic Association recommends 150 minutes a week of moderate to intense physical activity; these mind body activities can be considered moderate exercise. No real improvement in glycemic control was seen but beneficial effects on behavior, mood, stress, and quality of life were identified as positive outcomes (9). Because chronic stress has been implicated as an increased risk factor for the development of T2DM and we know stress induced inflammatory cytokines could be the cause of this finding, it is easy to see how daily practice of mind body medicine would have a positive effect. Many improvements have been documented with daily yoga training. Reduced fasting blood sugar and post-prandial levels, better glycemic control, and stable autonomic control are possible with daily yoga training.
Supplementation
Nutritional supplementation has been effective with diabetes management. As mentioned above various antioxidants are beneficial in preventing complications related to diabetes. The goal is to attempt to include as many fresh nutrient dense ingredients as possible and supplement as needed. High levels of oxidative stress have been found in diabetic patients, increasing the need for antioxidant supplementation. Deficient levels of vitamin C in diabetic patients are compounded by an impaired cellular uptake promoting hyperglycemia, which further decreases intracellular vitamin C levels. This localized deficiency contributes to end organ damage. Vitamin C supplements given at 1000 mg daily decreased urinary albumin and slowed the progression of diabetic nephropathy.
Electrolyte disorders have been found to play an important role in the complications of diabetes and are associated with increased mortality and morbidity. Several factors affect the bodies ability to utilize nutrients including; nutritional status, absorption, acid base imbalances, pharmacokinetics, renal disease, and acute illness. This might explain why diabetic patients are found to be low in several important nutrients. Hypomagnesaemia is commonly identified in diabetic patients. Magnesium is involved with more than 300 enzymatic reactions and is vital to glucose metabolism and insulin homeostasis. Low serum and plasma levels of magnesium are associated with alterations in nerve, muscle, and cardiac conduction. This contributes to nephropathy and end stage renal disease. Increased dietary intake of magnesium improved metabolic control and reduced the risk of T2DM and dyslipidemia (4).
The trace element chromium aids glucose with transport into the cell. Chromium deficiency induces hyperglycemia and impaired glucose tolerance. Normal chromium intake is <20 ug/day. Diet recall was used to determine the daily dietary intake of chromium. Low daily intake led to supplementing with 200 ug chromium picolinate or chromium rich yeast, which resulted in improved glucose tolerance. The findings held true in cases of gestational diabetes as well. Chromium is found in whole grains, broccoli, and grapes. Normal dietary intake ranges from 20-35ug/day, based on sex and age. Reduced HbA1c and fasting blood sugar levels were achieved with chromium supplementation. A large meta-analysis confirmed these results with a combination therapy of 600 ug chromium picolinide and 2 mg biotin (4).
Biotin is a B vitamin that enhances chromium absorption and is involved with intracellular metabolism of glucose. Biotin administration of 9-16 mg/day improved glucose tolerance and decreased mean fasting blood sugar by 45% (4). Inositol, D-chiro-Inositol and D-pinitol are found naturally in legumes and citrus fruits. D-pinitol mediates the action of insulin. When given at 20 mg/kg of body weight, a 5% decrease in plasma glucose is seen (4). Vitamin D deficiency has been associated with increased glucose tolerance and diabetes. Supplementation has shown improvement in endothelial function, glucose tolerance, and an increase in insulin secretion. Doses varied from 800- 300,000 IU/day (4).
a-Lipoic acid (ALA) is an antioxidant. One of its many benefits includes helping to avoid vitamin C and E deficiency which are important to prevent and treat T2DM. Supplementing with 600 mg of alpha lipoic acid effectively increased insulin sensitivity, slowed the progression of complications, and prevented renal damage in T2DM patients. ALA is naturally occurring in broccoli, brussel sprouts, peas, potatoes, and yeast (4).
Herbal Preparations
Bitter melon (momordica charantia) is a plant native to India and Asia. It has been used medicinally for over 600 years. Evidence has shown positive effects on glucose levels, glucose uptake, and glycogen synthesis and glucose oxidation (13). Active ingredients include charantin, vicine, and polypetide-p. Doses ranged from 150 and 2000 mg daily. Fruit, juice, and seed extracts were also used in some studies (12). Minimal side effects have been reported, although the ingredients are contraindicated in pregnancy. Four specific compounds identified provide the biological evidence for the benefits witnessed. An example of traditional or complementary medicine providing new and effective treatments for T2DM is metformin, which originated from goats rue (Galega Officinalis). Tan et al. identified bitter melon as one of the most popular botanical treatments for T2DM (14).
Another promising biologic T2DM treatment is Fenugreek, Trigonella foenum-graecum. Commonly used in Traditional Chinese medicine for glucose control, digestive aid, and relief of menopausal symptoms, Fenugreek given at 100 mg improved fasting blood glucose levels. Fifteen grams of ground fenugreek seed power with a meal lowered postprandial glucose levels (4).
Small trials have yielded promising results for Gymnema sylvestre or gurmar . The leaves of this plant are used in Ayurveda medicine to treat DM, cholesterol, and obesity. Significant improvement in fasting blood sugar and HbA1c levels were obtained with doses from 200 mg to 800 mg of an extract daily (4).
Cinnamon, Cinamonum cassia, gui zhi, Traditional Chinese Medicine, this differs from the common spice Cinnamonum verum. C cassia has been used for thousands of years to treat DM. The herb activates insulin receptors and increases glycogen synthesis. Five clinical trials evaluated doses from 1 – 6 grams daily and saw decreases in fasting blood glucose levels from 18 – 29 % (4).
Red Korean Ginseng was found to improve glucose tolerance test results, fasting plasma glucose, and blood sugar levels. American ginseng (AG) along with an herb called Konjac-Mannan (KJM) may improve T2DM control and associated complications. KJM affects the nutrient absorption rate in the small bowel while AG affects the post absorption activity, they work in unison to increase sensitivity and enhance secretion. Doses ranged from 100 – 200 mg BID reductions in fasting plasma glucose and HbA1c were documented (15).
Berberine is a compound found in golden seal, Oregon grape, barberry, and other plants. Some research as shown it to be as effective as metformin (16). Doses up to 1000 mg twice daily along with life style modifications lead to a 7% reduction in HbA1c. Glucose and lipid lowering properties were identified. Future T2DM treatment may have been identified by targeting free fatty acid metabolism.
Publication trends in Iranian endocrinology outlined highly cited articles effective in treating T2DM. Of the 44 articles found in PubMed, Scopas, and Google Scholar, a few of the relative topics include silybummarianum, Gaertn silyonarin, or milk thistle, as an effective treatment for T2DM and decreased serum glucose and HbA1c levels in diabetic outpatients using psyllium (4).
Shenyan Kangfu, based on Traditional Chinese Medicine and Zhao Enjian’s valuable therapeutic knowledge, is a traditional herbal preparation that has been improved and formulated into tablets. SYKFT tablets consist of 11 herbal ingredients with a synergic effect to nourish the kidney and spleen by detoxifying the body. Widely acclaimed shenya kangfu, has been used for DM nephropathy based on the qi-yin deficiency syndrome; swelling, fatigue, and weak limbs (25). Five sites in four major cities in mainland China have been identified. Enrollment is planned for 80 patients in stage III or IV diabetic nephropathy. Enrollment began in November 2012, 20 participants had been enrolled by March 2013 (17).
As outlined, there are many alternative treatments for T2DM that have been recognized as safe and effective. Small trials, meta-analyses, and anecdotal evidence provide recommendations and document safety concerns while outlining the need for additional research to improve the care that clinicians provide. The Natural Medicine Comprehensive Database confirms that many treatments outlined in this article are safe and effective. The U.S. Department of Health and Human Services contends that there is no high-quality evidence of benefit from alternative or supplemental treatments for diabetes. We as health care providers must use good judgment and available evidence to offer patients the best options for maintaining optimum health. Chandra and associates make it clear that we will never have absolute clarity on which therapies are effective and which are not. So much depends on patient preferences and available alternatives. He calls this the “gray zone” of medicine (18).
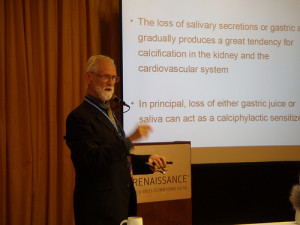
Chelation Therapy
Perhaps the most promising advance for the treatment of diabetes since insulin came from the Trial to Assess Chelation Therapy (TACT) (19). This trial emerged from a hearing of the Oversight committee of Congress and a subsequent call for proposals by the National Institutes of Health. TACT was designed to determine if future cardiac events could be reduced for patients at least 50 years of age who had already suffered at least one heart attack. It was a randomized, double-blind, clinical trial of 1708 patients, who were given more than 55,000 intravenous treatments. Half of the patients were given high dose vitamins. Thus there were four groups in the study: double placebo, high dose vitamins without chelation, chelation with placebo vitamins, and chelation with high dose vitamins (20). All of the patients were given evidence-based conventional care for their coronary artery disease. At the beginning of the five years that patients were followed, they were given 30 weekly IV’s and then 10 more treatments at monthly intervals.
The benefit of EDTA chelation was shown to be statistically significant. All of the cardiac events (death, re-infarction, stroke, coronary artery revascularization, and hospitalization for severe angina) were less in the EDTA groups than in the groups that received IV placebos. All cause mortality was also less in the treated patients. Further analysis showed that 37% of the patients had diabetes (322 EDTA and 311 placebo). For those patients with diabetes, there was a 41% reduction in cardiac events, a 52% drop in recurrent MI, and a 43% reduction in deaths. Those who received both chelation and high-dose vitamins had the best results, but even with chelation and placebo vitamins, the NNT for major cardiac events for diabetic patients over the 5 years was 6.5. For statins in such patients the NNT is considered to be highly effective at 17. Chelation was shown to be extremely safe when given according to protocol (18).
A major action of EDTA chelation is its removal of toxic heavy metals, such as lead, cadmium, arsenic, and mercury. Such metals are proven to be toxic to the vascular tree by their free radical activity (21). Carlos Lamar published numerous case studies in the mid-to-late1960 on chelation’s positive effects for diabetes (22). Paul Cutler found significant improvement in diabetic control with the use of the iron chelator, desferoxamine, in diabetic patients who also had high ferritin levels (23). EDTA also chelates iron, but not as effectively as desferoxamine. Therapeutic phlebotomies are more effective than either desferoxamine or EDTA. The vast majority of studies on chelation therapy and vascular disease were not randomized clinical trials and were of insufficient power to draw conclusions. Most of the studies did not identify patients who had diabetes.
The authors of TACT state that the magnitude of benefit for diabetic patients, calls for urgency to replicate their study (24). TACT-2 has been planned. At the same time, other forms of vascular disease, especially peripheral vascular disease, should be studied. Hancke and Flytlie published a remarkable study demonstrating that 24 out of 27 patients on the waiting list for amputation were able to cancel their surgery and save their legs (25).
Patient Decision-Making
In the meantime, TACT is clearly the best evidence available showing that chelation therapy might benefit vascular disease. The new guidelines for vascular problems call for the treating physician to have a conversation with his or her patients explaining the risks and potential benefits of all options of therapy. Then it is imperative that the patient decides what mode of therapy sounds best to him or her. This is the new “gold standard” (26). The patient is the decision-maker, not the doctor. Chelation therapy should be discussed in light of the evidence of TACT. If TACT-2 replicates TACT-1, chelation might be suggested for all diabetic patients. With the current status of evidence, chelation therapy should be offered to patients as an option for treatment, especially if they have signs of vascular disease.
Physicians trained in providing intravenous chelation report better overall results than TACT (27). One reason that clinical practice might be better is that continued monthly maintenance is commonly offered after the basic course of treatment. TACT treated patients intravenously only for the first 20 months, but followed them for 5 years. Another reason could be that TACT did not follow patients with challenge tests for heavy metals or vascular testing to assess progressive improvement. A re-accumulation of toxic metals is not unlikely. Finally, other nutritional therapies are often added by integrative physicians. All of these measures contribute to the best care for each individual patient and would likely improve the overall results.
Chelation therapy has been opposed by many conventional doctors for many years. In 1980, the AMA effectively said to the chelation community, “Put up some evidence, or stop doing the therapy”. With the help of NIH funding and cooperation among doctors familiar with the therapy and a group of courageous cardiologists, the evidence has arrived. As clinical scientists who continually advocate evidence-based medicine, physicians are obligated to accept good evidence when it conflicts with their beliefs (28). The rest of this article puts forth a comprehensive approach to diabetic patients that includes chelation therapy and alternative medicine as therapeutic options for prevention, control of the disease, avoidance of complications, and a longer lifespan.
A Comprehensive Integrative Approach to Diabetes
First, patients must realize it when they have either pre-diabetes or diabetes. This requires screening tests by their doctors’ orders or at health fairs, especially for anyone who is overweight or has a family history of diabetes. Patients with hypoglycemia not infrequently convert to diabetes as they grow older. Fasting blood sugars are a reasonable start but HbA1C tests are more accurate. Those who are overweight should be encouraged to eat less and better, and exercise more. Obesity is a major cause of gene expression into active diabetes.
As soon as pre-diabetes or diabetes is detected, a careful reassessment of lifestyle factors should be instituted. The patient and the family must embrace responsibility for controlling the disease. A healthy diet is crucial, with a special emphasis on low carbs if high triglycerides or the metabolic syndrome is present. Regular exercise and an effective way to deal with stress are important. Smoking and excessive environmental pollution are to be avoided as much as possible. Regular monitoring of lipids, HbA1C, kidney function tests such as creatinine with GFR and micro-albumen, vitamin D3 levels, annual eye exams, vascular screenings, and careful attention to the feet are all required. The sensitive CRP, homocysteine, and ferritin levels should be checked at least once. A challenge test is the best way to screen for toxic metals.
Nutritional supplements can help control the disease and avoid complications. Vitamin C, biotin, chromium, magnesium, zinc, selenium, B-complex, inositol, and alpha lipoic acid should all be considered. Several herbal supplements could also be selected if further control of the blood sugar is needed. Good candidates include cinnamon, bitter melon, and berberine. Fenugreek, Gymnema Sylvestre, Korean or American ginseng, KJM, and combinations of herbs from India or China also might have therapeutic benefit. Milk thistle might help by its detoxification of harmful chemicals. Psyllium is also good for detox, and aids constipation. Generally, herbals are safer and less likely to cause hypoglycemia than medications.
Medications are next on the list. Oral medicines are discussed above, and insulin is a reasonable choice if needed, whether or not the patient is insulin dependent. Doctors must be careful to avoid over-medication that can lead to HbA1C readings that are too low, hypoglycemic episodes, and severe injuries, especially in the frail elderly. Control of the disease is imperative. Therapeutic goals for the HbA1C should be 6.5-7.0 for most patients and 8.0 for unstable elderly patients. Of course, lower levels of HbA1C are desirable if they are achieved without the help of medications.
The most dramatic evidence of treatment success in the last few years came with TACT. Chelation therapy reduced future cardiac events and lowered the death rate for patients with diabetes who had a previous myocardial infarction. The magnitude of benefit was perhaps greater than any intervention other than considerable weight loss or insulin therapy. The probable mechanism has to do with free-radical activity and inflammation caused by toxic metals, which are removed with chelation. Confirmatory research is coming with TACT-2, but cardiologists and endocrinologists should at least describe the remarkable evidence generated by TACT-1 and let patients choose whether they want chelation, either before or after significant vascular disease has developed. After all, most of the complications from diabetes are vascular, which can lead to devastating disabilities and/or premature death.
References
- Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: U.S. Department of Health and Human Services; 2014.
- Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 2006; 444:840-846.
- Brand-Miller J, McMillan-Price J, Steinbeck K, Caterson I. Carbohydrates-the good, the bad and the whole grain. Asia Pacific Journal of Clinical Nutrition 2008;171 (Supplemental): 16-19.
- Gaby, AR. Endocrine disorders: Diabetes mellitus In Nutritional Medicine. Concord: Fritz Perlberg Publishing; 2011:1081-1105.
- American Diabetes Association. Standards of medical care in diabetes–2014. Diabetes Care 2014;37:14-80.
- Nelson JM, Dufraux K, Cook PF. The relationship between glycemic control and falls in the older adult. Journal American Geriatric Society 2007.
- 7. Lee SJ, Eng C. Goals of glycemic control in frail older patients with diabetes. JAMA 2011;305:1350-1351.
- DeMarco T. Bending towards integration: a mulltiple case studies assessing the progressive landscape of interprofessional collaborative care within U.S. integrative healthcare centers. Global Advances in Health and Medicine Journal 2013;2(Supplemental):1-2.
- University of Wisconsin-Madison. UW Health Integrative Medicine Updates Diabetes. Madison: UW Health Integrative Medicine and University of Wisconsin Department of Family Medicine 2005.
- Wendling P. Remote weight loss program works long term. Family Practice News 2011; 57.
- Esposito K, Maiorino MI, Petrizzo M, Bellastella G, Guigliano D. The effects of a Mediterranean diet on the need for diabetes drugs and remission of newly diagnosed type 2 diabetes: follow up of a randomized trial. Diabetes Care 2014; 37: 1824-1830.
- Perez-Martinez P, Garcia-Rios A, Delgado-Lista J, Perez-Jimenez F, Lopez-Miranda J. Mediterranean diet rich in olive oil and obesity, metabolic syndrome and diabetes mellitus. Current Pharmacutical Design 2011; 17: 769-777.
- Fuangchan, A. Sonthisombat, P, Seubnukarn, T, Chanouan, R, Chotchaisuwat, P, Siriguisatien, V, et al. Hypoglycemic effect of bitter melon compared with metformin in newly diagnosed type 2 diabetes patients. Journal of Ethnopharmacology 2011; 134: 422-428.
- Tan, MJ, Ye, JM., Turner N, Hohnen-Behrens C, Ke CQ, Tang CP, et al. Antidiabetic activities of triterpenoids isolated from bitter melon assocciated with activitation of the AMPK pathway. Chemical Biology 2008;15: 263-273.
- Vuksan V, Sievenpiper JL, Xu Z, Wong EY, Jenkins AL, Beljan-Zdravkovic U, et al. Konjac-Mannan and American Ginsing: emerging alternative therapies for type 2 diabetes. Journal Of American Collective Nutri 2001;10:370-380.
- Copeland A. A Study to determine the effectiveness of berberine Hcl on lowering HbA1c. The Original Internist 2014:171-172.
- Wang H, Mu W, Zhai J, Xing D, Miao S, Wang J, et al. The Key Role of Shenyan Kangfu tablets, a Chinese patent medicine for diabetic nephropathy: study protocol for a randomized, double blind and placebo-controlled clinical trial. Trials 2013;14:165.
- Chandra A, Khullar D, Lee TH. Addressing the challenge of gray-zone medicine. NEJM 2015; 372:203-205.
19.Lamas GA, Goertz C, Boineau R, Mark DB, Rozema T, Nahin RL, Lindblad L, Lewis EF, Drisko J, Lee KL. Effect of disodium EDTA chelation regimen on cardiovascular events in patients with previous myocardial infarction: the TACT randomized trial. JAMA 2013;309:1241-1250.
20.Lamas GA, Bouneau R, Goertz C, Mark DB, Rosenberg Y, Stylianou M, Rozema T, Nahin RL, Chappell, LT, et.al. EDTA chelation therapy alone and in combination with oral high-dose multivitamins and minerals for coronary disease: The factorial group results of the Trial to Assess Chelation Therapy. Am Heart J published by Mosby, Inc. as an open access article under the CC BY-NC-ND license, July 2014. Reprint requests from (gervasio)lamas@msmc.com.
21.Peguero JG, Arenas I, Lamas GA. Chelation therapy and cardiovascular disease: connecting scientific silos to benefit cardiac patients. Trends in Cardiovascular Medicine 2014: 232-240. Available on-line at www.sciencedirect.com.
22.Lamar CP. Chelation therapy of occlusive arteriosclerosis in diabetic patients. Angiology 1964;15:379-394.
23.Cutler P. Deferoxamine therapy in high-ferritin diabetes. Diabetes 1989, 38:1207-1210.
24.Escolar E, Lamas GA, Mark DB, Boineau R, Goertz C, Rosenberg Y, et.al. The effect of an EDTA-based chelation regimen on patients with diabetes mellitus and prior myocardial infarction in the Trial to Assess Chelation Therapy (TACT). Circ Cardiovasc Qual Outcomes 2014;7:15-24.
25,Hancke C. The long-term effect of chelation therapy: a 6-12 year follow-up of a 1993 study. Clin Pract Alt Med 2000;1:158-163.
26.Krumholz H.M. Variations in health care, patient preferences, and high-quality decision-making. JAMA 2013;311:151-152.
27.Chappell LT, Shukla R, Yang J, Blaha R, et al. Subsequent cardiac and stroke events in patients with known vascular disease treated with EDTA chelation therapy: a retrospective study. Evid Based Integrative Med 2005;2:27-35.
28.Maron DJ, Hlatky MA. Trial to assess chelation therapy (TACT) and equipoise: when evidence conflicts with beliefs. Published on-line from Mosby, inc. Department of Medicine, Stanford University. Email requests from david.moran@standford.edu. 2014