Blood viscosity and risk of cardiovascular events
Lowe GD1, Lee AJ, Rumley A, Price JF, Fowkes FG.
Abstract
We examined the relationships of whole blood viscosity and its major determinants to incident cardiovascular events (ischaemic heart disease and stroke) in a prospective study of a random population sample of 1592 men and women aged 55-74 years (the Edinburgh Artery Study). 272 fatal and non-fatal cardiovascular events occurred during 5 years of follow-up (cumulative incidence 17.1%). Age and sex adjusted mean levels of blood viscosity (3.70 v 3.55 mPa.s), haematocrit (46.2 v 45.7%), haematocrit-corrected blood viscosity (3.57 v 3.48 mPa.s), plasma viscosity (1.35 v 1.33 mPa.s) and fibrinogen (2.88 v 2.67 g/l) were significantly higher in subjects who experienced events than in subjects who did not. The relationships of these rheological variables to cardiovascular events were at least as strong as those of conventional risk factors (smoking habit, diastolic blood pressure, and low-density lipopr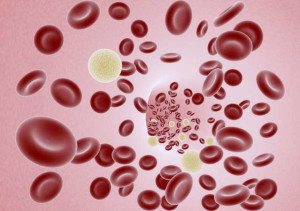 otein cholesterol). After adjustment for these conventional risk factors, the associations of blood viscosity and haematocrit remained significant for stroke, but not for total events; whereas the associations of plasma viscosity and fibrinogen remained significant for total events and for stroke. These findings suggest that increased blood viscosity may be one plausible biological mechanism through which increases in haematocrit and fibrinogen may promote ischaemic heart disease and stroke. Randomized controlled trials of viscosity reduction in the prevention of cardiovascular events (e.g. by lowering high levels of haematocrit or plasma fibrinogen) are suggested.
otein cholesterol). After adjustment for these conventional risk factors, the associations of blood viscosity and haematocrit remained significant for stroke, but not for total events; whereas the associations of plasma viscosity and fibrinogen remained significant for total events and for stroke. These findings suggest that increased blood viscosity may be one plausible biological mechanism through which increases in haematocrit and fibrinogen may promote ischaemic heart disease and stroke. Randomized controlled trials of viscosity reduction in the prevention of cardiovascular events (e.g. by lowering high levels of haematocrit or plasma fibrinogen) are suggested.